Liver cancer
- Oren Zarif

- Sep 3, 2024
- 17 min read
Updated: Feb 28
Treating Cancer
If you are dealing with cancer, I know exactly what to do.
I have thirty years of experience with thousands of success stories. My successes were reported in many media outlets; in addition, medical professors and doctors also benefit from my services.
My unique capabilities, as well as the energetic systems I have developed over many years can help you too.

Are you suffering from oncological problem?
Is your body struggling to recover?
It is a sign that the energetic fields in your body are blocked.
For years, Oren Zarif proved that as the energy blockades open, the body begins to create a healing process and returns to its strength. Thousands of patients testify about that. Many of those patients had suffered from oncological problems.
Therefore, it is important to open the body's blocked energy field channels for those patients who suffer from oncological problems. Only then, the body can cope with the existing problems and create a self-healing process.

With the unique method developed by Zarif over many years, and with his amazing capabilities, Zarif helped countless patients worldwide that had suffered from oncological problems
For 30 years Oren Zarif helped patients and sufferers around the globe who suffered from numerous and complicated problems
Oren Zarif became famous in all media channels in the country and worldwide throughout 30 years, among those channels: Sky News network, National Geographic and Fox network

If you are dealing with any kind of oncological condition, you have no reason to lose hope.
Leave your details here, and I will get back to you personally.
My treatment system receives custom approval procedures, and is delivered to each patient, anywhere around the globe.
The treatment is based on a completely energetic process, and is intended FOR EXTERNALUSE ONLY.
The reason that oncological conditions develop in the body stems from blockages in energetic channels, areas and conductors of the body.
Over many years, I have left even the most respected doctors, professors and scientists amazed, in front of my many successes with the most complicated
oncological cases from around the world.
My successes had been reported through several worldwide media channels.
hepatic cancer - energy healing technique
liver cancer - energy healing technique
liver metastases
liver tumor
hepatocellular carcinoma treatment
liver cancer - the body ability to heal itself
liver cancer - natural therapy
liver cancer - healing process
hepatic cancer - healing process
liver cancer - healing modalities
hepatic cancer - energy therapy
liver cancer - energy therapy
hepatic cancer - healing modalities
hepatic cancer - natural healing abilities
liver cancer - natural healing abilities
hepatic cancer - help the body heal itself
liver cancer - help the body heal itself
liver cancer
hepatocellular carcinoma
stage 4 liver cancer
hcc cancer
hepatocellular carcinoma treatment
liver cancer treatment options
hcc diagnosis
liver bile duct cancer
metastatic liver cancer
hcc liver cancer
liver tumor
liver metastases
liver cancer survival
hepatic cancer
liver carcinoma
liver cell carcinoma
secondary liver cancer
hepatic metastases
hepatic carcinoma
liver tumor treatment
liver cancer survival rates
primary liver cancer
adenocarcinoma liver
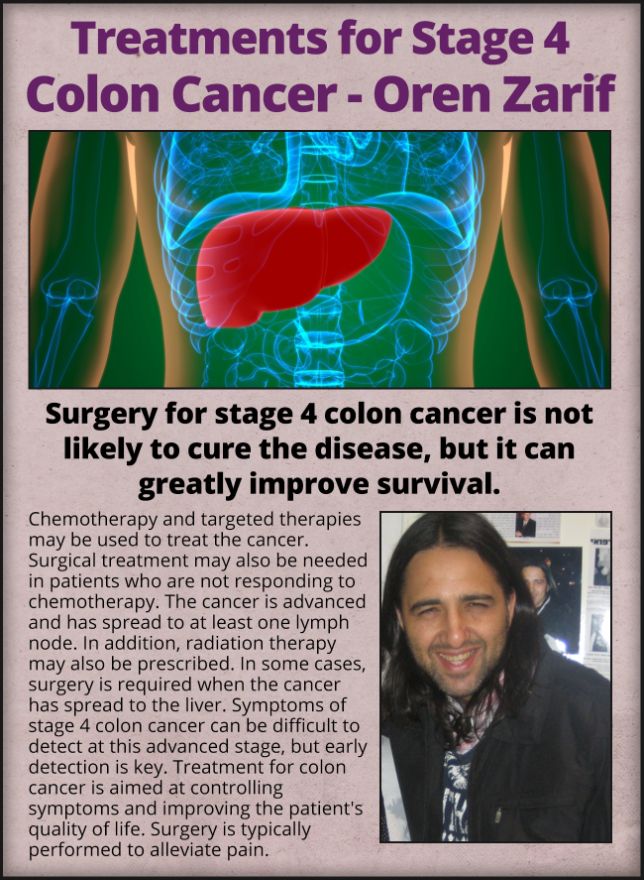
Factors That Increase the Risk of Liver Cancer
A number of factors increase a person’s risk for developing liver cancer. These include chronic infection with the hepatitis B virus and cirrhosis.
Hepatocellular carcinoma is the most common type of primary liver cancer. Other less-common types of liver cancer start in the bile duct cells, liver blood vessels or gallbladder cells (angiosarcoma).
Many of these tumors can be treated using minimally invasive techniques. These procedures use image guidance to deliver energy that freezes or heats the tumors and destroys them.
Hepatocellular Carcinoma (HCC)
Hepatocellular carcinoma (HCC) is a malignant tumor that arises from hepatocytes in the liver. It most often occurs in patients with cirrhosis caused by chronic viral hepatitis B virus (HBV) or hepatitis C virus (HCV) infection, but it may also occur in those without cirrhosis or other liver diseases. The incidence of HCC is rising worldwide, due to the increased endemic rates of hepatitis B and C infections.
A 71-year-old man was diagnosed with hepatocellular carcinoma after a liver biopsy demonstrated a mass in the right lobe of the liver that was suspicious for HCC. He had no history of liver disease or cirrhosis. The symptoms he experienced included pain in the right upper abdomen, abdominal swelling and bloating, fatigue, weight loss, and jaundice (yellow discoloration of the skin and eyes).
Benign liver tumors, such as cysts and hemangiomas, do not grow and are unlikely to cause any symptoms. On the other hand, hepatocellular carcinoma can grow rapidly and invade surrounding tissues or compress the main bile duct, internal organs, or large blood vessels in the abdomen, which can cause a variety of symptoms.
The most common symptoms of hepatocellular carcinoma are jaundice, abdominal pain and swelling, and itching. Other symptoms can include itching, nausea and vomiting, fever, fatigue, loss of appetite, and tiredness. Hepatocellular carcinoma is usually discovered as a result of a routine physical examination or other diagnostic tests such as blood and urine tests, magnetic resonance imaging (MRI), and computed tomography (CT). If liver cancer is detected, more detailed testing is performed to check if the cancer has spread to other parts of the body.
Most growths (tumors) in the liver are benign, which means they don’t contain cancer cells and will not become malignant in the future. Benign masses typically don’t require treatment, and many small ones can be monitored with regular imaging studies to make sure they don’t grow or cause symptoms over time. However, some of these masses may require further evaluation and possibly a liver biopsy to confirm they are not cancerous.
Focal nodular hyperplasia (FNH) is one of the most common types of benign liver tumors, and it often doesn’t cause symptoms. FNH can be diagnosed with US or CT imaging and is usually found incidentally. The characteristic appearance is a hypoechoic mass with displacement of vessels and a lobulated outline with a central scar. FNH can sometimes be mistaken for HCC, so it’s important to have the mass evaluated by a healthcare professional who has experience with this entity.
Hepatocellular adenoma (HCA) is another common benign growth that is usually found incidentally and can be associated with certain medications such as oral contraceptives or anabolic steroids. These growths are composed of sheets of liver cells (hepatocytes) and usually don’t compress the bile duct, portal vein, or hepatic lobule.
Liver hemangiomas are a more common type of vascular tumor and consist of tangled blood vessels in the liver. They are normally present at birth or develop in early childhood and don’t usually cause symptoms, but large hemangiomas can obstruct the hepatic duct or cause hepatic vein thrombosis. Occasionally, cavernous hemangiomas can be confused with metastatic melanoma and should be evaluated by a healthcare professional.
Some of these masses can be treated with minimally invasive techniques that destroy the tissue. Examples include radiofrequency ablation and microwave ablation, which involve applying heat to the tissue through a needle-like probe that kills the tumor cells. Other treatments include removing the entire tumor with surgical res
Liver Cancer Symptoms and Risk Factors
Cells in the liver grow, divide, and die on a regular schedule. Sometimes, these cells become cancerous and can spread to other parts of the body.
Liver cancer symptoms vary depending on where the tumor is and how much it ha
s spread. There are also several risk factors for developing cancer in the liver. Some of these risk factors can be changed.
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer. It develops in the liver and may spread to other organs.
The liver is the largest organ in the body. It performs many important functions, including metabolizing food and storing nutrients, making blood and clotting blood. It is also responsible for removing waste products from the body. Cancers can develop in the liver or spread to the liver from other parts of the body. Liver cancers are very common and the sixth leading cause of death worldwide. Hepatocellular carcinoma (HCC) is the most common type of liver cancer. It occurs in the main liver cells called hepatocytes. HCC most often develops in people with cirrhosis caused by chronic hepatitis B or C virus infection, but can occur in non-cirrhotic hepatitis and occasionally in healthy people.
The first signs of hepatocellular carcinoma may be pain in the abdomen and jaundice (yellowing of the skin and eyes). In later stages, cancer can lead to an enlarged liver or spleen, abdominal swelling (ascites), loss of appetite, fatigue and weight loss, confusion, fever, fatigue and weakness, and in severe cases liver failure.
Hepatocellular carcinoma is sometimes diagnosed at an asymptomatic stage, particularly in patients with small, asymptomatic tumors. Improved diagnostic techniques such as triphasic computed tomography scanning and magnetic resonance imaging have led to greater sensitivity and specificity in diagnosing hepatocellular carcinoma at an early stage.
Hepatocellular adenoma is a non-cancerous encapsulated structure that contains fluid. These tumors can be simple or complex, and most of them do not need to be treated. However, they can bleed or rupture. Extrahepatic cholangiocarcinoma is a rare form of cancer that begins in the ducts that drain bile from the liver into the intestine.
Hepatocellular carcinoma, also known as hepatoma, is cancer that starts in the liver. It is the most common type of primary liver cancer. Other types of primary liver cancer include hepatocellular adenoma and focal nodular hyperplasia, which are not usually biopsied. Other tumors in the liver that can mimic HCC include cholangiocarcinoma and metastatic deposits from extrahepatic primaries. These are often detected by imaging and may not be biopsied.
Cirrhosis is a condition that occurs when scar tissue replaces the healthy tissue of the liver. This scar tissue causes the liver to be unable to function normally and leads to complications such as hepatic failure, portal hypertension and jaundice. It also increases the risk of developing liver cancer and other tumors. Several factors can cause cirrhosis including viral hepatitis, liver disease and fatty liver disease.
Symptoms of cirrhosis include weakness and fatigue, itchy skin, stomach pain and bloating, vomiting and nausea, fluid retention (edema), bleeding in the abdomen (varices) and changes in mental status. Many people with cirrhosis don't have any symptoms and may not be diagnosed until their health is seriously deteriorating.
The diagnosis of cirrhosis is confirmed by a liver biopsy which is performed by inserting a needle into the liver to draw a small sample of tissue for testing. There are two major histological types of cirrhosis: micronodular and macronodular cirrhosis. In micronodular cirrhosis, regenerative hepatocyte nodules are scarcely larger than a normal lobular unit of parenchyma and are separated by thin connective tissue septa. In macronodular cirrhosis, the nodules are larger and more uniform than in micronodular cirrhosis.
Mixed cirrhosis is sometimes used as a term to describe the appearance of both micronodular and macronodular forms in the same patient at different stages of the disease. Generally, however, the term is not meaningful because it does not imply that these histological entities are mutually exclusive and can coexist in the same patient.
Some forms of cancer start in the liver cells (hepatocytes). The most common form is hepatocellular carcinoma, or HCC. This type of cancer usually affects men more than women and is most common in people over age 60. It’s also the fastest-growing type of cancer in the world.
In some cases, liver cancer can spread from another part of the body to the liver, a process called metastasis. This can happen when a cancer starts in the lungs or colon and then spreads to the liver. This type of cancer is treated the same as cancer that started in the liver.
Changes in Appetite or Digestion
Liver cancer may interfere with the way your body digests food, leading to changes in your appetite and digestion. This can include nausea, loss of appetite or abdominal pain. It can also lead to fatigue or weight loss. Unexplained itching is another possible symptom of liver cancer. This symptom is called pruritus. It may get worse
as the cancer gets more advanced.
Unusual Bleeding: Liver cancer can affect blood clotting factors, leading to abnormal bleeding. This can cause nosebleeds, excessive bruising or heavy or irregular menstrual bleeding in women.
Fatigue or Tiredness
Symptoms of liver cancer can make it hard to concentrate and feel like you have enough energy. This is because the tumor or cirrhosis can reduce your blood flow and oxygen supply to your brain.
Changes in Stool or Urine
Some types of liver cancer can block the production or release of bile, which makes your stool appear pale or clay-colored. It can also cause your urine to become darker or have a deeper amber color. These symptoms are usually a sign of more advanced liver cancer and should be brought to the attention of your doctor.
Hepatocellular Carcinoma
Primary liver cancer starts in the liver cells (hepatocytes). It is most commonly caused by hepatitis B or C virus infection and
Hepatocellular carcinoma can acquire atypical “parasitic” vascular supply from extra-hepatic arterial pedicles recruited by the tumor. Such a finding must be recognized on pre-treatment CT scan or arteriography before chemoembolization.
Hepatocellular carcinoma is a malignant neoplasm of epithelial liver cells. It may be well differentiated with uniform tumor cells indistinguishable from normal hepatocytes or a more poorly differentiated neoplasm with pleomorphic, irregular cells. It is associated with chronic hepatitis B virus infection and some types of cirrhosis.
The diagnosis of hepatocellular carcinoma is typically made by ultrasound and CT scan, and occasionally by MRI. Liver biopsy is recommended for tumors that are large (>3 cm in diameter) or symptomatic. Hepatocellular carcinoma is more common in cirrhotic than in non-cirrhotic liver disease, but it can also occur in healthy livers. It is important to distinguish HCC from benign hepatiocellular adenoma and focal nodular hyperplasia, and to identify metastatic deposits from extrahepatic primaries (eg, intrahepatic cholangiocarcinoma) and other primary cancers of the liver such as biliary cancer and angiosarcoma.
It is essential to establish the vascular anatomy of hepatocellular carcinoma before chemoembolization. The majority of hepatocellular carcinomas are vascularized from the hepatic artery, and this should be clearly identified on the pre-treatment CT scan or arteriography. It is also possible for hepatocellular carcinomas to acquire "parasitic" vascularization from extra-hepatic arteries recruited to the tumor, and this needs to be recognized on CT or MR images before chemoembolization.
Many other tumors of the liver or hepatic sinuses can appear "hepatoid" under the microscope, and these should always be considered in the differential diagnosis of hepatocellular carcinoma. These include hepatocellular adenocarcinoma of bile ducts, gallbladder carcinoma spreading into the liver, epithelioid hepatocellular carcinoma of the pancreas, clear cell renal carcinoma, and gastrointestinal stromal tumor.
The liver is a large organ in the upper right side of the abdomen. It has two main functions: to store nutrients from food and to break down and remove harmful chemicals from the body. It also builds chemicals that the body needs to stay healthy. Cancer develops when cells in the liver grow out of control. There are many types of liver cancer. The most common type of liver cancer is hepatocellular carcinoma (HCC).
HCC starts in liver cells called hepatocytes. It occurs most often in people with cirrhosis from long-term use or viral hepatitis. However, it can also occur in people with non-cirrhotic chronic liver disease,
A person with hepatocellular carcinoma may have no symptoms, or they might experience nausea and vomiting, abdominal pain and jaundice (yellowing of the skin and whites of the eyes). The tumor may grow rapidly, causing liver failure. If hepatocellular carcinoma spreads to other parts of the body, the signs and symptoms will change and become more severe.
There are four stages of hepatocellular carcinoma, and the symptoms get worse as the cancer progresses.
The first sign of hepatocellular carcinoma is a pain in the right side of the belly. A person may also feel tired or weak, and might have a yellowing of the skin and eyes (jaundice). People with hepatocellular carcinoma may have high levels of a protein in the blood called alphafetoprotein (AFP), which is made by immature liver cells.
A person with hepatocellular carcinoma that has not yet spread to other parts of the body may be treated by having surgery to remove the tumor and part of the liver. Surgical removal may be combined with chemotherapy or other treatments. The AFP level in the blood is usually measured again after chemotherapy, to see if the cancer has reduced. If the cancer has not recurred, it is possible to have regular follow-up visits and have blood tests done to check for the presence of the tumor and to monitor fo
Many types of tumours can develop in the liver. Most of these are benign (not cancerous). Some of them don't need treatment if they're small and not causing symptoms. Others may need treatment to control the spread of the tumour or prevent it from becoming more serious. Hepatocellular carcinoma is the most common type of primary liver cancer. It develops from the main liver cells, called hepatocytes. It usually occurs in people with cirrhosis.
Hepatocellular carcinoma can also be vascularised in other ways. It may be supplied by a hepatic artery in up to 2.2% of patients [8]. It can also be vascularised in the postero-inferior part of the right lobe by the superior renal capsular artery, which branches from the inferior adrenal artery. The intercostal arteries can also be used to supply tumors in the anterior peripheral subcapsular area of the liver. These can be visualized on multidetector CT scans and can be targeted with hepatocellular carcinoma chemoembolization.
Hepatocellular carcinoma occurs in most cases as a consequence of chronic hepatitis B and/or hepatitis C virus (HBV and HCV) infection leading to cirrhosis.
Considering the relatively limited therapeutic efficacy of treatment options in advanced HCC, prevention is an attractive strategy for improving patient prognosis. Multiple preventive strategies have been suggested including vaccination against HBV and/or HCV, dietary control of aflatoxins and other toxins associated with contaminated food products, hepatitis-associated fibrosis suppression and maintenance of normal liver function through nutritional support.
In addition, there is growing interest in the use of noninvasive methods for hepatocellular carcinoma early detection. For instance, circulating tumour DNA (ctDNA) based assays can monitor for cancer cell signalling pathways and predict whether a patient is likely to develop hepatocellular carcinoma.
Stage 4 Liver Cancer
A cancer’s stage is an important metric for predicting how it will respond to treatment. It’s based on how many people with a particular type and stage of cancer live five years or longer.
Immunotherapy has shown promise in treating HCC, but only for a small subset of patients. This is why it’s important to have a diagnosis and begin treatment as early as possible.
Stage 4 Cancer
A cancer that starts in the liver is called primary liver cancer. There are 5 main types of primary liver cancer, but the most common is hepatocellular carcinoma (HCC). This type of cancer develops in liver cells called hepatocytes. It often happens when the liver has long-lasting damage from hepatitis virus infection or cirrhosis. HCC is more common in men and people over the age of 60.
In stage 1 of hepatocellular carcinoma, the tumor is small and hasn’t spread to nearby blood vessels. Symptoms of this stage may include jaundice and abdominal pain or discomfort. Liver cancer that is in this early stage can often be treated with surgery and radiation.
For people with hepatocellular carcinoma, the survival rate drops significantly in stage 4. In this stage, the tumor is larger and has spread to nearby tissues or blood vessels. People in this stage often have severe symptoms, such as fatigue and weight loss. They also have high chances of developing bile duct obstruction.
Hepatocellular carcinoma in this advanced stage is often diagnosed by imaging tests. CT and ultrasound images can reveal enlarged areas of the liver, which is known as hepatomegaly. The cancer may also be visible as a nodule on an imaging test.
The stage of the cancer is determined by how large the tumor is, whether it has invaded other parts of the liver, and if it has spread to lymph nodes. It’s important to know the staging of the cancer because it can help your doctor choose the best treatment option for you.
A biopsy can confirm a diagnosis of stage 4 liver cancer. A biopsy can show that the liver cancer is poorly differentiated, which means it has a lot of similarities to normal liver tissue. It can also show if the cancer has a cirrhotic architecture.
There are several treatment options for people with advanced liver cancer. Some of these treatments target specific genes, proteins, or the environment that supports cancer growth. Others, such as immunotherapy, boost the body’s natural ability to fight cancer. Palliative care, which focuses on comfort and pain relief, can also be helpful for people with advanced liver cancer.
Stage 4 Metastasis
A metastatic liver cancer is when the cancer has spread beyond the liver to other parts of the body. This can happen either when the cancer cells escape from the liver through the bloodstream or when the cancer develops from a non-cancerous (benign) tumor that then metastasizes to other organs or tissues.
The most common type of liver cancer is hepatocellular carcinoma, or HCC. It usually develops in people with chronic (long-lasting) liver disease caused by hepatitis virus infecti
on or cirrhosis. The disease affects more men than women, and it is the sixth leading cause of cancer death in the United States. It’s also the most common cause of cancer in people who live in America’s Native American or Alaska Native communities.
Metastasis is a dangerous condition that can significantly reduce survival rates. Cancers that meetastasize can grow and invade surrounding tissue, resulting in liver failure or even liver death. It is not uncommon for a patient to have multiple metastases at the time of diagnosis.
There are many different kinds of metastatic liver cancer. It can be challenging for health care providers to determine which treatments will be effective for a given patient. Often, these treatments are based on the patient’s overall medical history and other factors such as age and disease stage.
One of the most important things for a patient to know is that survival rates for a specific cancer or its stage can change frequently. They can be influenced by new research, changes in treatment options or even the results of other studies. Therefore, it is important for patients to stay up-to-date with their treatment plans and to see a doctor regularly.
Researchers are studying how different components of the liver interact with each other to influence cancer development. For example, one team is investigating how the liver’s fatty composition can alter the way in which cancer cells function. The study shows that cancer cells may use metabolites derived from fat to weaken anti-tumor immunity.
Another group is examining the ways in which a tumor’s vascular expansion and aggressiveness are controlled. They are using multiparametric liver imaging, liquid biopsy technologies, big data science and mathematical modelling to better understand these interactions.
Stage 4 Treatments
The liver is the largest solid internal organ in the body and performs hundreds of critical functions, includi
ng filtering toxins, processing nutrients, storing glucose and regulating blood clotting. Liver cancer can start in the primary liver cells known as hepatocytes or in the surrounding fat, connective tissue and blood vessels that support the liver. The most common type of liver cancer is hepatocellular carcinoma, which accounts for three-fourths of all diagnoses.
Hepatocellular carcinoma may spread to other parts of the body. It can spread to the bile ducts, other organs of the liver, the gallbladder and the lungs. Other types of liver cancer include cholangiocarcinoma, which starts in the lining of the bile ducts, and angiosarcoma, which occurs when tumors grow from blood vessels in the liver.
Once a diagnosis of stage 4 liver cancer is made, your care team will create a treatment plan tailored to the type of cancer you have and its location in your body. A personalized approach to treatment can help improve your chance of survival and quality of life.
Your treatment plan will depend on the size and location of your tumors, whether the liver cancer has spread and what types of treatment you are receiving elsewhere in your body. Some of the treatment options for stage 4 liver cancer are surgery, radiation therapy, immunotherapy and treatments.
Stage 4 Care
When the cancer reaches stage 4, it's usually too late to cure it with surgery or other treatments that would have been effective in earlier stages. At this point, doctors focus on reducing symptoms and prolonging life. They work with a team of specialists called an interdisciplinary team.
A group of experts in different fields will meet to discuss your care and make decisions about your treatment. They might also refer you to a specialist or recommend palliative care.
If you have hepatocellular carcinoma, the cancer that starts in liver cells (hepatocytes), your doctors will assess the condition's clinical and pathological stages. This is based on physical examination, biopsy results and imaging data.
HCC is the most common type of primary liver cancer. It can develop in any age and gender but is more common in people over 60. It is also more common in men than in women and gets worse with advancing age.
Symptoms of hepatocellular carcinoma usually don't appear until bile flow is blocked, which causes jaundice. This is characterized by yellowing of the skin and whites of the eyes, itchy skin, pale stools and black urine.
The medical community is developing new strategies to treat advanced liver cancer. Scientists are focusing on the role of cancer stem cells in the progression of liver tumors. They are finding ways to prevent the formation of these cells and destroy them. This approach could lead to the development of more effective therapies to treat stage 4 hepatocellular carcinoma.
Researchers are studying ways to block the secretion of molecules that promote cell proliferation in hepatocellular carcinoma and other malignant tumors. These molecules, known as microvesicles, are released by cancer stem cells during epithelial-to-m
esenchymal transition. They also contribute to tumor invasion and metastasis.
Some patients with hepatocellular carcinoma in the early stages may benefit from minimally invasive treatments that deliver chemotherapy directly to the tumor. One example is chemoembolization, which involves injecting small particles that contain chemotherapy to block the arteries that feed the tumors while sparing healthy liver tissue. Another minimally invasive treatment that the Hershey Medical Center team uses is radioembolization with Y-90, which involves inserting a catheter into the hepatic artery and then infusing it with smaller particles that contain radiation to target the hepatocellular carcinoma.
liver tumor treatment
liver metastases
hemangioma liver
hepatic carcinoma
liver metastases treatment
liver lesions cancer
liver and pancreatic cancer
hepatocellular cancer treatment
hepatic cholangiocarcinoma
liver metastasis treatment
neuroendocrine tumor liver
aggressive liver cancer
curing liver cancer
cancer in your liver
treatment for advanced liver cancer
melanoma in liver treatment
treatment for liver lesions
liver sarcoma
hepatic angiosarcoma
angiosarcoma liver
hepatic adenoma treatment
angiosarcoma liver treatment
liver malignancy
carcinoid liver cancer
spread to the liver
sarcoma liver cancer
cancer in bones and liver
if you have liver cancer
multiple hepatic metastases
adenocarcinoma spread to liver
.png)























































































Doesn’t say contact details
Hallo my dr. Told me got 2 years live i have cervical then went to liver this year also got blood clog clove to heart well my dr. Dr from heart said I'm fine but still got that problem and my colon got hurt when they did radiation and chemo well left it weak that it bleed all time that dosent let me get chemo well new chemo is tvdak that's new chemo she's going start me with please help